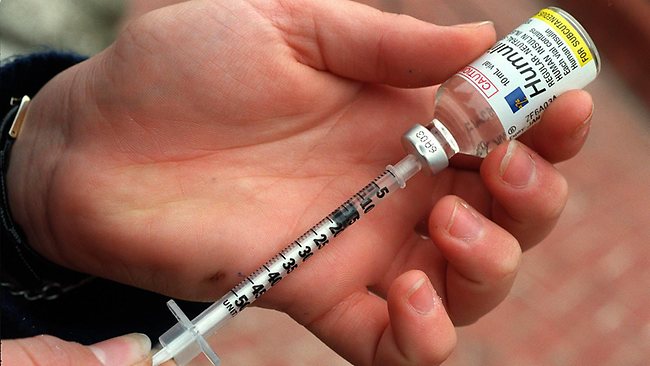
Insulin Injections and Diabetes – A Love Hate Relationship
Categories: Diabetes, Medications, Weight Loss
Do you want to gain weight? Inject yourself with insulin and you will surely accomplish that goal. It does not matter if you are diabetic or not, insulin signals our fat cells to absorb food energy and make us fat.
On the short term insulin therapy might help to regulate blood sugars, but over the long haul insulin therapy is rather costly to our health as it is fattening, inflammatory and can worsen other chronic diseases like atherosclerosis and heart disease.
This is not to say that insulin therapy should be avoided altogether, it is just a matter of appropriate use. The American Diabetes Association (ADA) guidelines for years have pushed the use of insulin therapy in type 2 diabetic patients without much regard to endogenous (pancreatic) insulin production and more importantly proper diet.
Indeed, we cannot live without insulin. There is an absolute need for insulin, to the tune of 50-100 units or less per day depending on diet. Normally the pancreas can handle insulin production. The problem with type 2 patients is that insulin receptors become resistant to the insulin signal and the pancreas struggles to keep up with insulin demand. Eventually the pancreas loses its ability to produce insulin. It is at this point where insulin therapy makes sense.
The problem we often see (based on ADA guidelines) is patients starting insulin therapy prematurely despite a functioning pancreas. Long term these patients gain weight and require more and more insulin. On high carbohydrate standard American diets (SAD), patients and healthcare professionals have few medical options.
Let us stop this insanity. The only way to reduce insulin requirement is to reduce the consumption of carbohydrates in the diet, period!
I cannot tell you how frequently I see overweight type 2 patients who are taking massive amounts of insulin to the tune of 150-250 units per day. The story is always the same. They all gained weight with the initiation of insulin therapy, especially the short acting varieties.
Teach patients how to eat low carb high fat (LCHF) foods, they lose weight and overnight insulin requirements are cut in half. Insulin resistance and type 2 diabetes are metabolic disorders caused by dietary carbohydrates and insulin overload. Insulin injection therapy is not the answer and should only be reserved for type 1 and type 2 patients who no longer produce endogenous insulin.