Who’s the cholesterol expert now?
Categories: Cardiovascular Risk Assessment, Cholesterol, Scientific Evidence & Research
My new chemical engineer friend and colleague, Ivor Cummins, has turned biochemistry into his hobby. Although I can think of many more entertaining hobbies it is fascinating to watch Ivor use his engineering skills, calculating his way through piles of evidence to solve the nutrition, cholesterol and health equation. Listen and watch his technical but fascinating presentation, The Cholesterol Conundrum – and Root Cause Solution:
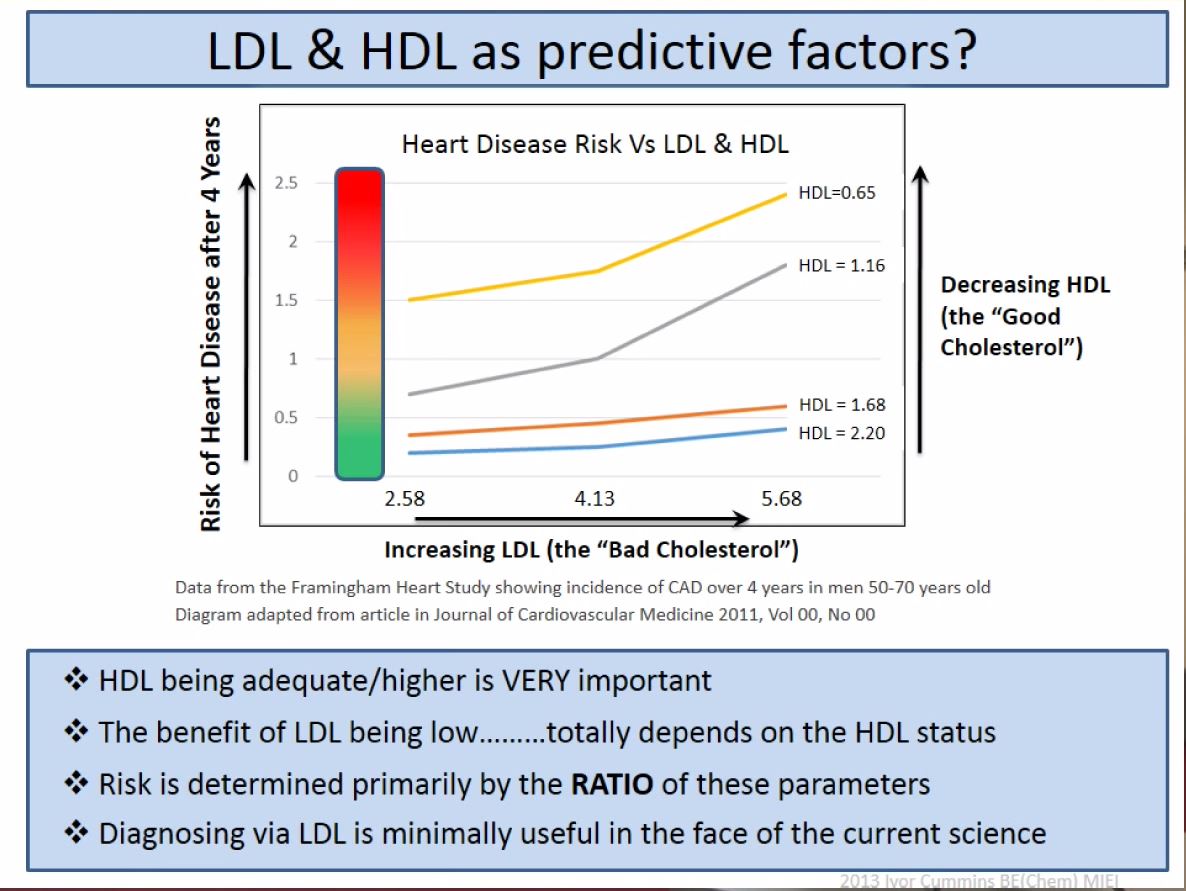
My favorite slide and discussion starts at around 45 minutes into the presentation, looking at LDL-C relative to HDL-C. Direct observation from the Framingham heart study data: LDL-C does NOT predict cardiovascular risk as HDL-C rises (see the image below using international units mmol/l).
In other words, LDL-C becomes mostly irrelevant as HDL-C improves! To date ONLY a nutritional approach, specifically a well formulated low carb high fat (LCHF) diet reduces risk by raising HDL-C, and lowering triglyceride, consistent with the favorable markers observed in the original Framingham study. We also now know that LCHF diets favorably improve cholesterol size and quality regardless of LDL particle count/concentration (a surrogate measurement to LDL-C), based on modern advanced NMR lipid testing.
Good luck Big Pharma finding a blockbuster drug for this one. BTW, Mother Nature figured this out long ago!
It’s unfortunate that decades of research, based on mostly weak evidence and unproven hypotheses, leaves mainstream to believe that lowering LDL-C via low fat, low calorie diets or cholesterol medication is the only way to reduce risk. Mainstream needs to better understand nutrition including whole foods diets and how to critically look at the evidence (or lack of it).
I hope to collaborate with Ivor and applaud his well done effort.